
How does diabetes affect the feet?
Diabetes is a chronic condition that can have widespread effects on the body, and one of the most overlooked areas it impacts is the...
Read morePain is a complex experience controlled by the nervous system and influenced by physical, psychological, and social factors. When your body becomes injured, specialized nerve endings called nociceptors detect potential harm and send signals to the spinal cord and brain. The brain then interprets and assesses these signals, deciding whether or not to produce the sensation of pain. However, this system is not always perfect. Pain can be amplified or persist even after an injury has healed, or it can occur in the absence of any injury at all. This is due to the over-protective nature of our body’s alarm system for pain.
The brain’s interpretation of pain is influenced by various factors, including past experiences, emotions, expectations, and environmental cues. For example, if someone has had a previous injury in a certain area, they may be more sensitive to pain in that region even if there is no new damage. Additionally, the brain can “learn” pain over time, meaning if someone is in pain for a long period of time, it becomes the normal state of being whereby the body doesn’t know any difference other than a pain state. This can lead to heightened sensitivity even when the original cause is no longer present. This experience can be referred to as ‘hyperalgesia’ where the increased sensitivity to feeling pain provokes an extreme pain response. This is particularly common in chronic pain conditions. Another phenomenon some people may experience is ‘allodynia’, which occurs when a pain is caused by a stimulus that doesn’t usually cause pain such as clothing on skin, or water running over an extremity.
Conditions like lower back pain or fibromyalgia often involve persistent pain despite no new / ongoing tissue damage.
People who have had limbs amputated can still feel pain in the missing limb, showing that pain is not solely dependent on physical injury.
High levels of stress, anxiety, or lack of sleep can make pain feel worse, even if there is no physical injury present.
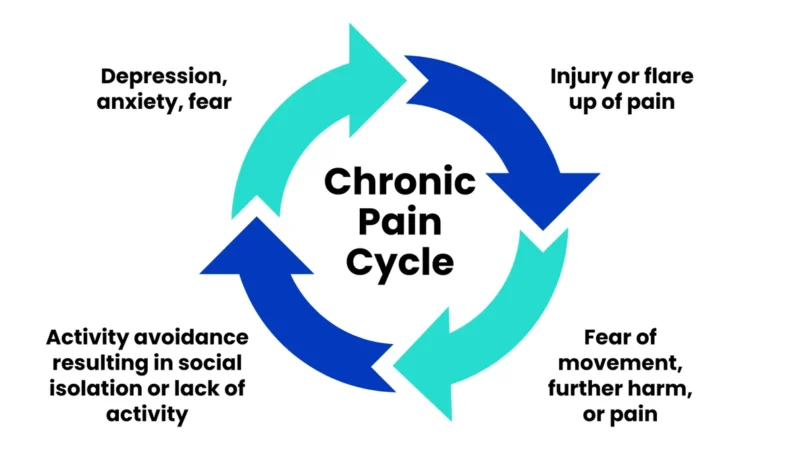
Stress can significantly increase the perception of pain due to its impact on the nervous system. When the body is under stress, it enters a state of heightened alertness, known as the “fight-or-flight” response. This leads to an increase in stress hormones like cortisol and adrenaline, which can amplify pain signals by making the nervous system more sensitive. Chronic stress can also cause prolonged muscle tension and inflammation, and reduced blood flow, all of which have potential to contribute to increased pain levels. When stress impacts the normal function of the brain, it can be more challenging for the body to regulate and dampen pain signals when they arise. Over time, this creates a cycle where pain leads to more stress, which in turn exacerbates the pain experience. This repetitive pain cycle is something we often notice in athletes who have recurrent exacerbations of pain and find it challenging to move out of pain and into the prevention phase of their journey.
Experiencing pain doesn’t necessarily mean you are making an injury worse or creating more damage. It’s important to understand that pain is influenced by many factors, including emotions, past experiences, and even social conditioning. Learning how to identify safe, realistic levels of pain during rehab from an injury compared to pain from actual damage can help reduce fear associated with exercise and improve overall well-being.
Avoiding movement due to the fear of pain can actually slow down recovery in most cases. While it may feel uncomfortable at first, gentle and gradual movement can help retrain the nervous system to see that exercise is safe and that it can actually help improve circulation, and restore function. Working with a physiotherapist can help you safely reintroduce movement depending on your injury and build confidence in your body’s ability to heal.
Addressing lifestyle factors like stress, sleep, and mental health can play a big role in managing persistent pain. Techniques such as mindfulness, meditation, deep breathing exercises, and stress management strategies can positively influence the way pain is perceived. Additionally, seeking support from a physiotherapist or other healthcare professionals can provide guidance tailored to your specific needs.

All of our PEAK physiotherapists can confidently assess your pain, determine whether there is any tissue damage, and guide you through a tailored recovery plan. This might include gentle movement, strengthening exercises, dry needling or active release techniques, education about pain, and strategies to retrain your nervous system’s response to pain. They are also able to help identify when you could benefit from being referred onto other healthcare professionals for help, such as sports doctors, specialists, occupational therapists or psychologists.
If you’re struggling with persistent pain, book an appointment with one of our friendly PEAK coaches to understand what’s really happening in your body and how to move forward with confidence!

Diabetes is a chronic condition that can have widespread effects on the body, and one of the most overlooked areas it impacts is the...
Read more
Pain is often perceived as a warning sign that something is wrong in the body. While this can be true in cases of an...
Read more
Choosing His Pain Lleyton, one of our dedicated physiotherapists, recently crossed the finish line of the Tokyo Marathon in 5 hours and 20 minutes—a remarkable...
Read more
Finding the perfect running shoe can often feel like a challenge—there’s an overwhelming number of options to choose from, and it’s hard to know...
Read more
Insights into PEAK Coach Callum’s Journey! The road to the marathon is no easy feat, but for many, it’s a bucket list item worth the...
Read more
How Women’s Health Physiotherapy Can Support Your Birth Experience Pregnancy is a time of incredible change and anticipation, and as you approach your birth day,...
Read more
With summer drawing to a close, and taking the stinking hot days with it, for many of us that signals the start of the...
Read more
Acute wry neck is a common musculoskeletal condition characterized by sudden and severe neck pain, often accompanied by abnormal head positioning and muscle spasms....
Read more
And the role Physiotherapy can play in managing it. Joint hypermobility is a very common presentation that our clinicians treat at PEAK and it is...
Read more
Meet Luke, a PEAK athlete with a story we have all heard before – lower back pain that leaves you completely debilitated for days. Luke...
Read moreNot exactly what you're looking for?
View all articles
















Can't find what you're after?
View all ServicesOr email the PEAK team at info@peakssc.com.au
To make a booking outside of business hours, please use our form by clicking here.
To make a booking outside of business hours, please use our form by clicking here.